Cardiac Arrest
Adult Basic and Advanced Life Support
Author: Emily Hillman, MD, Assistant Professor Emergency Medicine, University of Missouri-Kansas City
Editor: Julianna Jung, MD, Department of Emergency Medicine, Johns Hopkins University School of Medicine
Introduction
More than 300,000 out-of-hospital cardiac arrests occur each year in the United States and approximately 10% survive the arrest.1,2,3 Around 200,000 in-hospital cardiac arrests occur every year and about 20% survive to hospital discharge.3 4,5 Basic
life support (BLS) is critical to saving lives. High-quality CPR and early defibrillation can dramatically improve survival.6
Objectives
Upon completion of this self-study module, you should be able to:
- Describe the BLS and Advanced Cardiac Life Support (ACLS) Survey critical actions
- Discuss the importance of adequate chest compressions and early defibrillation in the management of pulseless patients
- Develop a list of common emergent causes for patients presenting with cardiac arrest
- Explain the initial evaluation and key management strategies for patients with cardiac arrest
- Identify asystole, ventricular tachycardia and ventricular fibrillation on an ECG
- Identify heart block and paroxysmal supraventricular tachycardia on an ECG
- Describe the initial treatment of asystole, pulseless ventricular tachycardia, ventricular fibrillation and pulseless electrical activity
- List the most common causes of pulseless electrical activity and their treatments
Initial Assessment
The 2010 American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care (ECC) changed the BLS sequence to emphasize the importance of early chest compressions with the mnemonic C-A-B (compressions, airway, breathing).2The 2015 AHA Guidelines Update for CPR and ECC recommends that in order to reduce time to first chest compression, trained rescuers should simultaneously check for breathing and circulation, and initiate CPR if a pulse is not definitively identified within 10 seconds.7
High-quality CPR and defibrillation are priorities when caring for a patient in cardiac arrest. Early defibrillation is critical to patient survival. The time from cardiac arrest to defibrillation is one of the most important determinants
of survival: for witnessed ventricular fibrillation (VF) arrest every minute without defibrillation survival rates decline by 7-10%. If high-quality CPR is performed this decline in survival is slowed.8
BLS Survey: Early CPR & Early Defibrillation2,7,8
- Recognize cardiac arrest
- Check responsiveness
- If unresponsive, perform CAB assessment by simultaneously assessing circulation, airway, and breathing (<10 seconds) (Tip: Check the carotid pulse while visually observing for chest rise and normal breathing)
- No pulse and no normal breathing
- Activate the emergency response system and send someone to get an automated external defibrillator (AED)
- Initiate chest compressions without delay
- Begin chest compressions and ventilations with the following ratios: (Tip: Begin compressions first. Unless asphyxia caused the arrest, blood is fully oxygenated at the time of arrest; it is only once oxygen is depleted the breaths become essential.
Compressions circulate blood flow to the heart, lungs, and brain. Without blood flow, oxygen cannot be provided to the organs.)
- No advanced airway: breaths provided via bag-mask device in a ratio of 30 compressions to 2 breaths
- Advanced airway: continuous compressions and 1 breath every 6 seconds
- Defibrillate
- Should occur as soon as the AED arrives
- As indicated per AED or rhythm analysis (for information on shockable and non-shockable rhythms see below). (Tip: An AED will only shock ventricular tachycardia and ventricular fibrillation, which are both “shockable” rhythms)
- Immediately resume CPR after defibrillation. If no shock is indicated, resumed CPR immediately
- Reassess
- Every 2 minutes (or 5 cycles of CPR)
- Every 2 minutes (or 5 cycles of CPR)
High-Quality CPR: Best Practices
- Hand Placement: 2 hands on the lower half of sternum. (Tip: Place the heel of one hand on the midline of the chest approximately 4 finger fingerbreadths above the xiphoid process. Place the other hand on top.)
- Key Actions7,8,9
- Push hard (Tip: The use of a backboard and/or stepstool may be required maximize compression depth and allow full recoil.)
- Depth of 2 inches but no more than 2.4 inches
- Allow complete chest recoil between compressions
- Push fast
- 100-120 compressions/minute
- Pushing faster than 120/minute compromises depth7
- Minimize pauses in compressions
- Less than 10 seconds
- Only for rhythm checks and defibrillation
- Switch providers every 2 minutes or 5 cycles of CPR
- Ventilate adequately
- 2 breaths after 30 compressions.
- Deliver each breath over 1 second.
- Each breath should cause chest rise. (Tip: Only deliver enough tidal volume to produce visible chest rise, avoid excessive ventilation)
- Push hard (Tip: The use of a backboard and/or stepstool may be required maximize compression depth and allow full recoil.)
High-quality CPR is the single most important determinant of survival for patients with cardiac arrest. Performing CPR according to the above guidelines optimizes blood flow to major organs.9 Up to 30% of baseline cardiac output is generated by properly performed CPR.10 Cardiac output is determined by stroke volume and heart rate.
Cardiac Output (CO) = Stroke Volume (SV) x Heart Rate (HR)
Compression rate directly affects cardiac output, while compression depth determines stroke volume. Inadequate depth and rate reduces cardiac output. The changes in intra-thoracic pressure that are created by high-quality CPR optimize venous return and forward blood flow, thereby improving cardiac output.
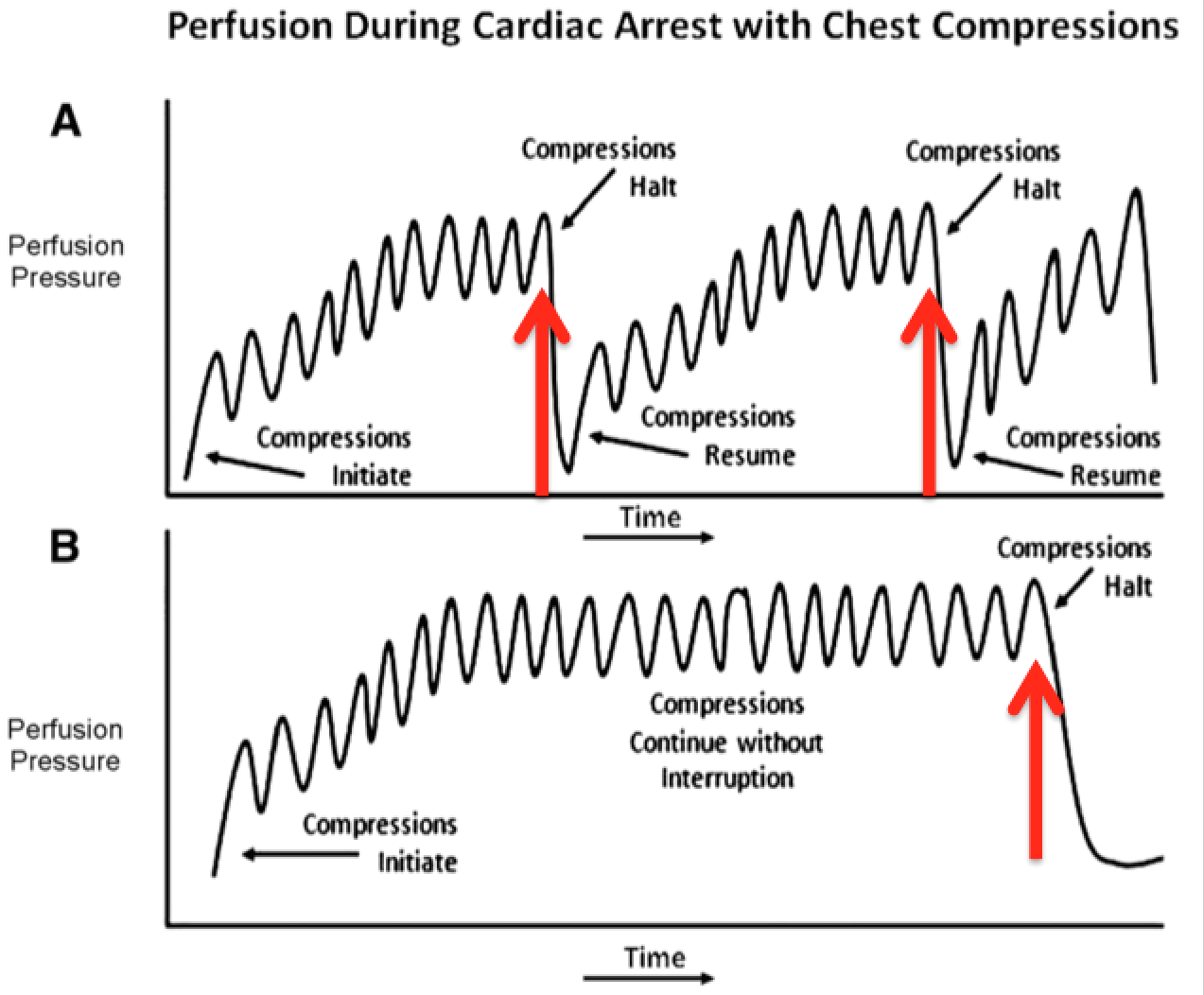
Compression rate and depth are the most common errors of resuscitation during cardiac arrest and both errors may reduce the likelihood of survival.6 Stopping compressions stops blood flow to the heart and brain; minimizing interruptions provides consistent blood flow.11 Figure 111 below illustrates the importance of minimizing pauses in compressions.
Assessment of Airway and Breathing
The BLS survey focuses on patients without a pulse and without normal breathing. A rapid pulse and breathing assessment enables providers to quickly determine if a patient is in arrest and begin chest compressions. When assessing an airway, the goal is to determine its patency. A patient who is awake and talking normally has a patent airway and is unlikely to need emergent intervention. An unresponsive patient without a gag reflex or with pooling secretions will need emergent intervention. A head tilt-chin lift or jaw thrust can be used, however frequently a nasopharyngeal airway (NPA) or oropharyngeal airway (OPA) is required.
Most arrest victims will not breathe normally, though some gasps or agonal respirations may be noted peri-arrest. If a pulse is present but there is not symmetric full chest rise, then breathing may be inadequate. You must support the breathing
using a bag-mask to deliver 1 breath every 5-6 seconds or insert an advanced airway. The decision to insert an advanced airway depends on the clinical situation, provider skills, and the environment.
ACLS Survey: Identify & Treat
- Circulation
- Assess: CPR quality, presence or absence of a pulse, cardiac rhythm, need for defibrillation or cardioversion (Tip: Remember to only pause CPR to assess the rhythm and pulse every 2 minutes.)
- Intervention: provide defibrillation when indicated (ventricular fibrillation/tachycardia), obtain vascular access, administer medications and/or IV fluids as indicated.
- Airway
- Assess: patency
- Intervention: head tilt-chin lift, OPA, NPA (Tip: sometimes a two-person technique will necessary to maintain an open airway to provide high-quality bag-mask ventilation. http://lifeinthefastlane.com/ccc/bag-mask/)
- Insert advanced airway if needed (Literature: Good bag-mask device technique will enable ventilation in most cases. Inserting an advanced airway does not provide a survival benefit. Provider skill and experience should be considered7,12)
- Breathing
- Assess: chest rise (Tip: Due to poor perfusion during cardiac arrest you may not be able to rely on skin color, O2 sat, and CO2 as a measure of adequate ventilation)
- Intervention: 100% oxygen (arrested patient)
- May require going back to airway
- Defibrillation
- Based on rhythm (for information on shockable and non-shockable rhythms see below)
- Dose: 200J biphasic
- Reassess
- Every 2 minutes (or 5 cycles of CPR)
Rhythm Identification and Treatment
Sometimes health providers use the word “shock” when referring to either defibrillation or cardioversion. While both therapies involve delivery of electricity to the heart, they are physiologically distinct and have different indications. Defibrillation is the random administration of a shock (an electrical current) that is not synchronized with the QRS complex. Cardioversion is the timed administration of a shock that is synchronized with the QRS complex. The electrical current provided by the shock causes the myocardium to contract and interrupt the arrhythmia, giving the sinus node an opportunity to resume normal activity.10
Not all patients in cardiac arrest benefit from defibrillation, which is why the ACLS protocol distinguishes between shockable and non-shockable rhythms. Patients in asystole and pulseless electrical activity (PEA) do not respond to defibrillation.
This is because in PEA there is already an intrinsic rhythm, so defibrillation doesn’t “add” any benefit. In asystole the myocardial cells are not responsive due to lack of intrinsic myocardial activity.10
Shockable Rhythms
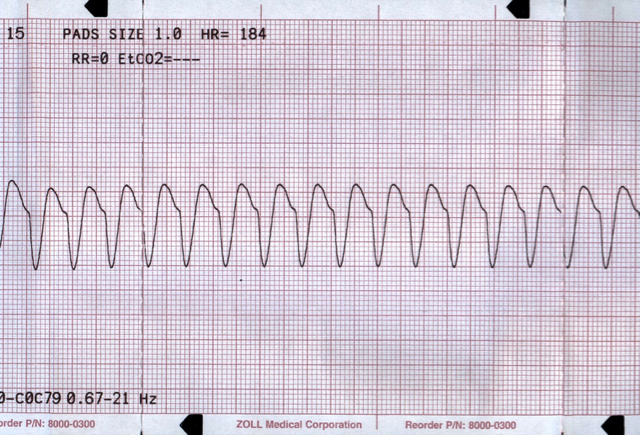
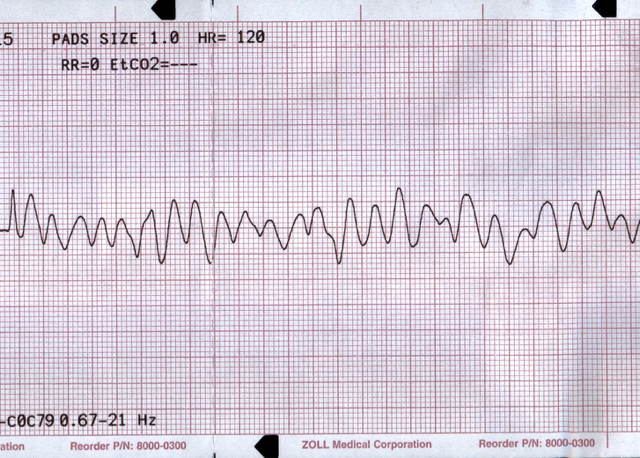
Pulseless Ventricular Tachycardia (VT)
- Rate typically exceeds 120-130/minute but is usually ³ 180/min
- Absence of P and T waves
- Wide (> 120 milliseconds) and regular QRS complexes
Acute myocardial infarction and structural heart disease are the most common underlying causes of VT.10
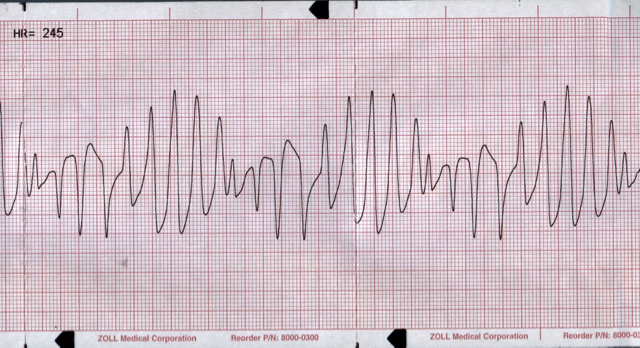
Pulseless Torsades de Pointes (“Twisting of the Points”)
- A specific type of polymorphic VT associated with QT-prolongation
- Rate typically 180 – 250/min
- Absence of P and T waves
- Wide QRS complexes with varying morphology and amplitude
- Certain drugs (tricyclic antidepressants, procainamide, some antihistamines to name a few) and electrolyte abnormalities (hypokalemia, hypocalcemia, hypomagnesemia) can cause QT-prolongation.8
Ventricular Fibrillation
- Disorganized
- Absence of P and T waves as well as QRS complexes
Treatment VT/Pulseless Torsades/VF
- High quality CPR
- Early defibrillation
- Medications (Literature: Antiarrhythmic medications for cardiac arrest have not been shown to increase survival after cardiac arrest12)
- Epinephrine 1mg 1:10,000 dilution, IV push every 3-5 minutes (Literature: In 2015 vasopressin was removed from the adult cardiac arrest treatment algorithm.7)
- Amiodarone: 1st dose 300mg IV bolus. 2nd dose 150mg IV bolus
- Magnesium (for torsades de pointes): 1-2grams IV diluted in 10mL normal saline over 30-60 seconds
Non-Shockable Rhythms
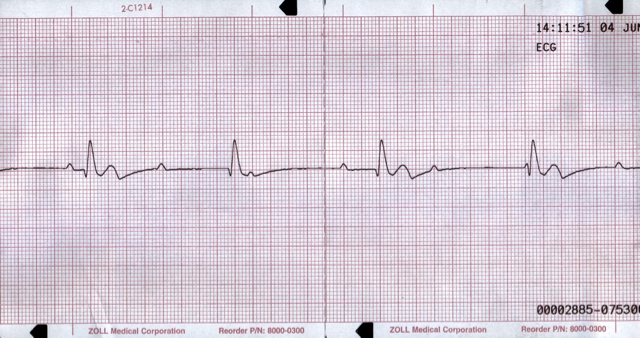
Pulseless Electrical Activity
- Presence of an organized or semi-organized rhythm
- No appreciable pulse
- Excludes ventricular tachycardia, ventricular fibrillation and asystole
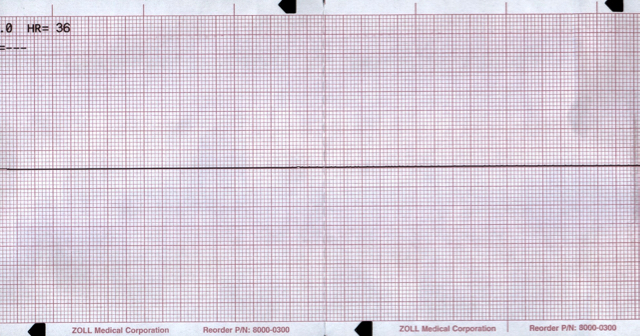
Asystole
Asystole is the absence of electrical activity, confirmed in at least 2 leads (Tip: assumes equipment functioning properly; check to ensure all monitor leads are properly attached to the patient and the monitor.)
Treatment PEA/Asystole
- High quality CPR
- Epinephrine 1mg IV every 3-5 minutes (Literature: In 2010 atropine was removed from the adult cardiac arrest treatment algorithm2.)
- Search for and treat underlying reversible causes
Differential Diagnosis for PEA Arrest
Identifying and treating the underlying cause for the arrest may improve patient survival. The following is a list of potential reversible causes of cardiac arrest and some considerations for treatment.6 Each of the reversible causes listed can result from a variety of disease conditions. A good history and physical exam can help you focus your rapid assessment and is extremely important.
When considering how the underlying causes might lead to cardiac arrest it is helpful to consider the underlying pathophysiology. An acute myocardial infarction (AMI) or a massive pulmonary embolism (PE) can cause acute heart failure or cardiogenic shock leading to profound hypotension. Similarly, certain toxins can cause myocardial dysfunction or peripheral vascular dilation resulting in hypotension.2 Severe dehydration or massive blood loss cause hypovolemia and can can lead to hypotension. When left untreated, the result is a profoundly decreased (non-palpable) blood pressure in the presence of a visible rhythm on the monitor, hence the term pulseless electrical activity.
| Reversible Cause | Differential | Evidence/Work-up | Treatment/Intervention |
| Hypovolemia | Dehydration, sepsis, hemorrhage | History (volume or blood loss, fever)
Physical exam (pallor, poor skin turgor, rectal bleeding)
Bedside ultrasound (IVC measurement, RUSH exam | IV fluids
Blood products |
| Hypoxia | Airway obstruction, pulmonary disease/pathology causing impaired oxygenation | History (past medical problems, recent respiratory illness, risk factors for pulmonary embolism)
Physical exam (abnormal breath sounds, leg swelling)
O2 sat (if detectable) | Basic airway maneuvers or interventions. Advanced airway placement |
| Hydrogen ion (acidosis) | Acidosis is usually not the primary cause of arrest | History, ABG | Ensure adequate ventilation, sodium bicarbonate |
| Hypokalemia (HypoK) or Hyperkalemia (HyperK) | Volume loss, renal failure, other electrolyte | History (dialysis, recent vomiting or diarrhea)
Physical exam (AV fistula)
Electrocardiogram (EKG) | Magnesium and potassium (hypoK)
Calcium chloride, glucose and insulin, sodium bicarbonate (HyperK) |
| Hypothermia | Environmental | History
Physical exam (cool skin, central temperature)
EKG | Active and passive warming techniques |
| Trauma | Pneumothorax
Cardiac Tamponade | History
Physical exam (JVD, tracheal deviation, chest wall crepitus, absence of breath sounds)
Bedside ultrasound (E-FAST^) | Tube thoracostomy (Pnuemothorax) Pericardiocentesis (Tamponde) |
| Toxins | Drug Overdose | History
Physical exam (presence or absence of diaphoresis, pupillary response and size) | Antidotes |
| Thrombosis | Pulmonary embolism
Acute coronary syndrome (ACS) | History, EKG, bedside ultrasound | Thrombolytics or embolectomy (PE)
Percutaneous coronary intervention (AMI) |

Post Cardiac Arrest Care
When caring for patient post cardiac arrest, consider reversible causes. The following is a list of assessments and interventions that should be performed after return of spontaneous circulation (ROSC):2,7
- Maintain adequate ventilation and oxygenation
- Ensure O2 sat ≥ 94%
- Ensure waveform capnography
- Consider advanced airway
- Optimize hemodynamics (treat systolic blood pressure <90 mm Hg or mean arterial pressure <65 mm Hg). (Tip: not all patients will benefit from both IVF and vasopressors in the setting of hypotension. A consideration of the perceived cause of
arrest, presenting rhythm, and bedside assessment of the patient’s volume status and ventricular function can better help delineate.)
- IV fluids with a 1-2 liter bolus of normal saline or lactated ringer’s
- Vasopressors: consider epinephrine, dopamine, or norepinephrine (Tip: consider in patients presenting in VF/VT arrest; VF/VT are associated with cardiac events that can lead to cardiogenic shock.)
- Consider targeted temperature management
- Comatose patients
- Target temperature: 32°C-36°C for at least 24-hours
- Fever prevention is acceptable
- Assess for acute coronary syndrome
- 12-lead EKG
- Consider coronary angiography
References
- CPR & Sudden Cardiac Arrest (SCA) Fact Sheet. (2014, September 3). Retrieved June 3, 2015 from http://www.heart.org/HEARTORG/CPRAndECC/WhatisCPR/CPRFactsandStats/CPR-Statistics_UCM_307542_Article.jsp
- American Heart Association Emergency Cardiovascular Care Committee. (2010). 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 122:S639–946. doi: 10.1161/CIR.0b013e3181fdf7aa
- Heart Disease and Stroke Statistics—2015 Update A Report From the American Heart Association. (2014). Circulation, 131, E29-E322. doi:10 .1161/CIR .0000000000000152
- Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: Incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33(2):237-245.
- Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39(11):2401-2406. (Epidemiologic registry study, 433 patients)
- Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JME, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Sampson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF. Part 1: executive summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(suppl 2):S315–S367. (Circulation. 2015;132[suppl 2]:S315–S367. DOI: 10.1161/CIR.0000000000000252.)
- American Heart Association Emergency Cardiovascular Care Committee. (2015). Highlights of the 2015 American Heart Association Guidelines Update for CPR and ECC (Ebook ed., pp. 1-33). American Heart Association.
- Sinz, E., Navarro, K., & Soderberg, E. (Eds.). (2013). Advanced Cardiovascular Life Support Provider Manual (EBook ed., pp. 11-213). Dallas, TX: American Heart Association.
- Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, Gazmuri RJ, Travers AH, Rea T. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(suppl 2):S414–S435. (Circulation. 2015;132[suppl 2]:S414–S435. DOI: 10.1161/CIR.0000000000000259.)
- Mahadevan, S., & Garmel, G. (Eds.). (2012). An Introduction to Clinical Emergency Medicine (2nd ed., pp. 41-49). Cambridge: Cambridge University Press.
- Rezaie, S. (2015, March 15). Epinephrine in Out-of-Hospital Cardiac Arrest Poll. Retrieved June 4, 2015, from http://rebelem.com/epinephrine-in-out-of-hospital-cardiac-arrest-poll/
- Link, M. S., Berkow, L. C., Kudenchuk, P. J., Halperin, H. R., Hess, E. P., Moitra, V. K., . . . Donnino, M. W. (2015). Part 7: Adult Advanced Cardiovascular Life Support. Circulation, 132(18 suppl 2). Retrieved February 4, 2016, from http://circ.ahajournals.org
- Hampton, J. (2013). The ECG Made Easy (8th ed., pp. 1-83). Churchill Livingstone Elsevier.
- Grauer, K. (2014). ECG Pocket Brain Expanded Version (6th ed.). Gainesville, Florida: KG/EKG Press.